Client: male, Age: 25, Diagnosis: Anxiety. His anxiety has been increasing over the past few weeks. Social: lives with his parents, works as a software engineer. Medical: no significant medical history. Goals: to reduce anxiety and improve sleep.
SOAP Note Generator
Generate SOAP notes for tracking and documenting client progress.
 HIPAA Compliant: Our platform is fully HIPAA compliant, ensuring your healthcare data is protected with the highest security standards.
HIPAA Compliant: Our platform is fully HIPAA compliant, ensuring your healthcare data is protected with the highest security standards.Harness AI to dramatically speed up your content creation
Our AI-powered tool can generate high-quality, tailored content in seconds, not hours. Boost your productivity and focus on what really matters.
Use Cases
Discover how this template can be used in various scenarios
Healthcare Providers
Documenting patient encounters with structured SOAP notes that meet clinical documentation standards.
Mental Health Professionals
Creating detailed therapy session notes while maintaining client confidentiality and treatment progress.
Physical Therapists
Recording patient assessments, treatments, and progress using the SOAP format for rehabilitation services.
Nurse Practitioners
Maintaining comprehensive patient records with organized SOAP documentation for primary care visits.
Medical Students
Learning and practicing proper clinical documentation through structured SOAP note writing.
Occupational Therapists
Tracking client interventions and outcomes with detailed SOAP notes for therapy sessions.
How to use the SOAP Note Generator
SOAP Note Templates & Examples
Frequently asked questions
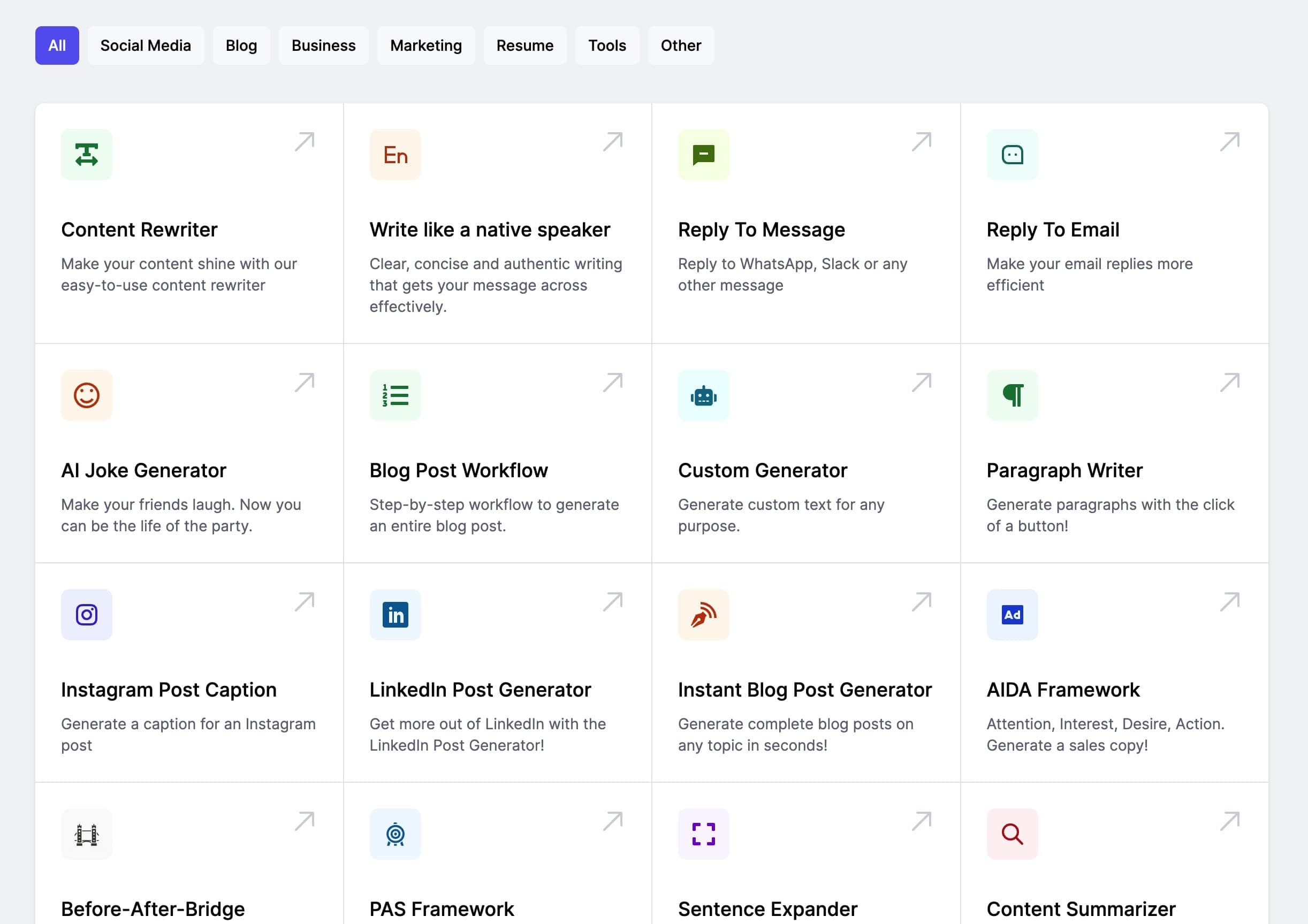
Check out these other templatesSee all →
Psychotherapy Progress Note Generator
Generate progress notes for tracking and documenting client progress in therapy sessions.
Generate comprehensive BIRP (Behavior, Intervention, Response, Plan) notes for mental health professionals.
Clear, concise and authentic writing that gets your message across effectively.
Create Faster With AI.
Try it Risk-Free.
Stop wasting time and start creating high-quality content immediately with power of generative AI.