Garrett is a 20 year old white male living at home with his parents and his younger brother Elliot (19). Garrett is experiencing significant stress due to the transition from high school to adult life, exacerbated by a history of anxiety and autism. He has struggled with anxiety throughout their life and began medication in third grade, which initially helped but has since worsened with recent life changes. He has previously sought therapy for suicidal thoughts and feelings of helplessness. Family history of psychiatric issues includes ADHD and anxiety in a sibling, and ADD in a mother, all of whom are medicated. Garrett is currently on Vyvanse, Escitalopram, and Guanfacine. There are no reported substance use or legal issues. Engagement with parents and friends has been supportive during this transition.
Therapy Intake Generator
Generate a comprehensive therapy intake note including client background, presenting concerns, history, risks, and goals.
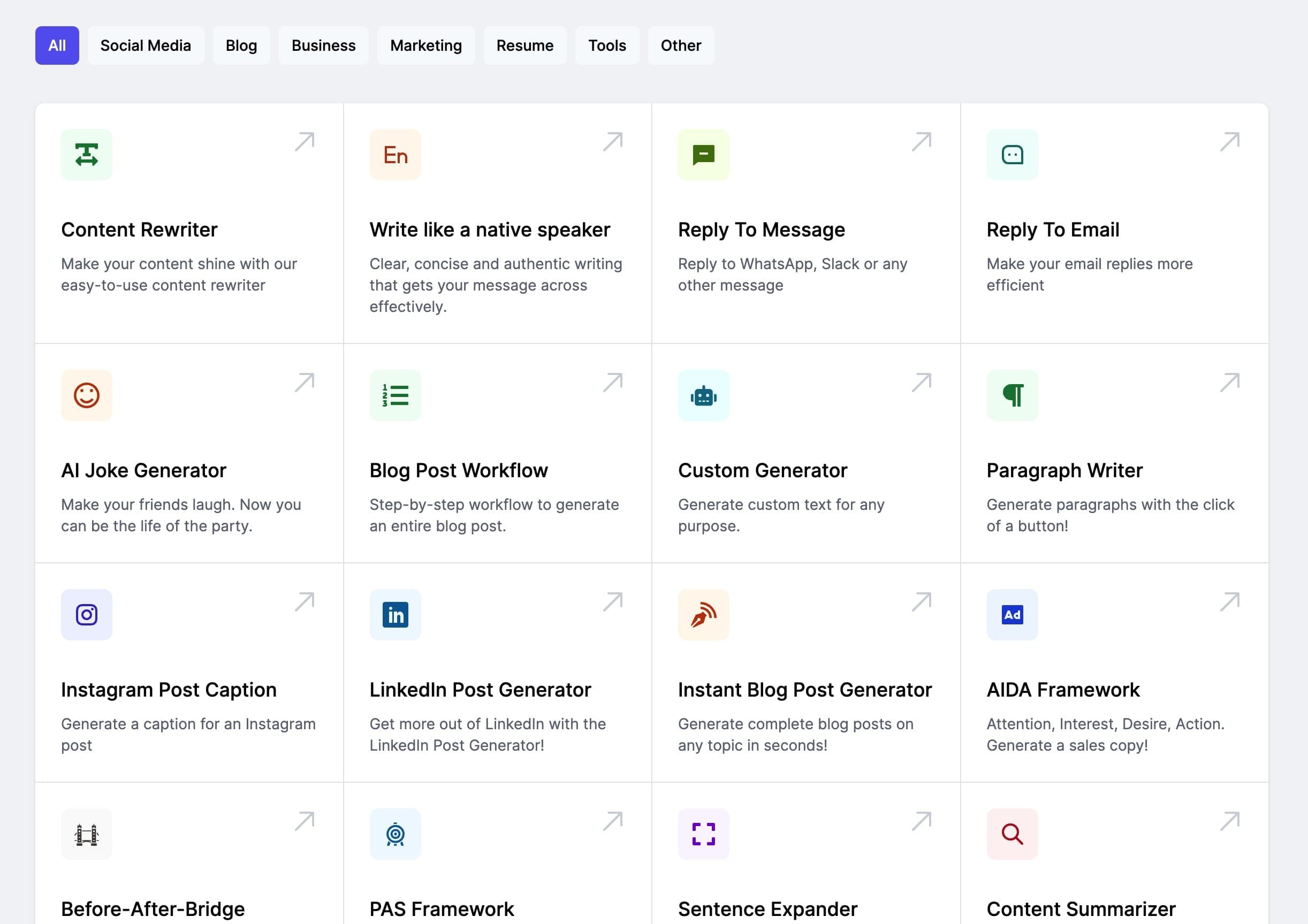
Harness AI to dramatically speed up your content creation
Our AI-powered tool can generate high-quality, tailored content in seconds, not hours. Boost your productivity and focus on what really matters.
How to use the Therapy Intake Generator
Therapy Intake Templates & Examples
- INPUTOUTPUT
- INPUT
William is an inmate at the Wood County Jail and is presenting counseling as a participant in the Wood County Jail Recovery Pod program. William reports that he has been at the jail for approximately one month and that he is in the recovery pod as an alternative to the revocation of his probation through he WI Department of Corrections. William reports that he has a history of drug abuse, specifically heroin, and that he has been incarcerated in the majority of his adult life, beginning at age 16 when he states he was sentenced to precision as an adult William is 37 year old, native American he grew up in California, moved to Wisconsin when he was 14, he Has been incarcerated the majority of his adult life.
OUTPUTTherapy Intake Note
1. Identifying Information and Reason for Visit:
Client Name: William
Age: 37
Gender: Male
Cultural Identity: Native American
Date of Intake: [Insert Date]
Setting: Wood County Jail Recovery Pod
Referral Source: Self-referred as a participant in the Wood County Jail Recovery Pod Program to avoid the revocation of probation through the Wisconsin Department of Corrections.
Reason for Visit: William presents with concerns related to past substance abuse, mental health symptoms, and difficulties adjusting to jail dynamics, particularly feelings of being bullied in the cell block.
2. Presenting Problems:
Onset and Duration: Issues with substance abuse began in childhood; incarceration has been a recurring theme since age 16. Current incarceration has lasted for approximately one month.
Triggers: Interpersonal conflicts and feelings of bullying within the jail environment contribute to his distress.
Severity: Reports significant distress from perceived bullying, fear of aggression leading to expulsion from the recovery pod, and the ongoing battle with substance use.
Functional Impact: Struggling to maintain composure in a challenging environment; previous attempts to achieve sobriety have been unsuccessful.
3. Psychosocial History:
Family/Supports: William has a complex family history, having been raised by a mother with substance use issues and having experienced abuse by his aunt and uncle. He has a significant other, Kristi, whom he considers his wife; their relationship is a source of motivation.
Education/Work: Completed high school while incarcerated; has experience running a screen printing business. Has taken various vocational classes in prison.
Living Situation: Currently residing in the recovery pod at the jail; has faced instability due to incarceration.
Cultural Factors: Identifies strongly with Native American culture; expresses that it is an important aspect of his life and recovery journey.
4. Relevant Medical and Psychiatric History:
Previous Diagnoses: Previously diagnosed with "bipolar schizophrenia"; current understanding aligns with schizoaffective disorder, bipolar type.
Prior Treatments: Hospitalized involuntarily three times as a juvenile; prescribed medications including Geodon, Lithium, Risperidone, and Risperdal with varied effectiveness.
Current Medications: Currently on Suboxone (16mg daily) for opioid use disorder; previously on Vyvanse.
5. Substance Use:
History: Initiated substance use at age 9 with exposure to meth and heroin; self-reports long-standing addiction issues, particularly with heroin.
Current Status: In recovery pod as part of a mandated program; demonstrates insight into the need for sobriety.
6. Risk Assessment and Safety Plan:
Self-Injury/Suicidal Ideation: William denies any current or past suicidal ideation or self-harm behaviors.
Access to Means: Incarceration limits access to means for harm; currently supervised in a controlled environment.
Protective Factors: Willingness to seek help; desire for a stable relationship with Kristi and to lead a sober life.
7. Clinical Impressions and Provisional Diagnosis:
Clinical Impressions: William presents with a complex interplay of mental health symptoms, substance use disorder, and external stressors related to his current environment.
Provisional Diagnosis: Schizoaffective Disorder, Bipolar Type; Opioid Use Disorder.
8. Client Goals and Initial Treatment Plan:
Client Goals:
To maintain composure and avoid aggressive responses to bullying.
To achieve sobriety and work towards a happier life, particularly for the sake of his relationship with Kristi.
Initial Treatment Plan:
Frequency: Weekly sessions during incarceration.
Modalities: Cognitive-behavioral therapy to address coping skills, psychoeducation about schizoaffective disorder, and substance use recovery strategies.
Homework/Next Steps: Explore triggers related to feelings of bullying; develop personalized coping strategies. William will identify positive reaffirmations he can use when facing conflicts.
Next Appointment: [Insert Date and Time]
Therapist Signature: [Your Name, Credentials]
Date: [Insert Date] - INPUT
Identification:Morgan is a 17 year old, white male who lives on a hobby farm in Milladore with father Chris (54), mother Kathy (49), sister Golda (12), and brother Gus (20), as well as several animals. Morgan has his own room.
Has concerns with his family entering his space without knocking
Trauma History:History of corporal punishment from mom "belt, stick, Medical Conditions & History:Underweight for his age. No other concerns repoted at intake. Current Medications:Prescribed duloxetine 30 mg and aripiprazole 2 mg Substance Use:No issues reported at intake. Family History:Morgan is reported to have a close relationship with to his aunt Heather and uncle Steve. Morgan reports his relationship with sister Golda (12) is “not the best”, however, it has improved. Morgan reports that he gets along with his older brother Gus (21), who also lives in the home. Morgan has described his relationship with his mom as “iffy” and “good” with his dad.
Dad plays Warhammer with Morgan to develop their relationship
Morgan is very isolated and describes himself as an introvert Scared that his parents will kick him out of the house when he turns 18 Social History:Morgan stated "I have not been the most social person; I want to be more social, more outgoing." Morgan is close to his neighbor Jack who is similar aged, and he states that the majority of his peer interactions are online/ virtual. Spiritual/Cultural Factors:No spiritual beliefs beliefs Developmental History:Speech and maybe dyslexia, Educational/Vocational History:Does online schooling,- - Attended online school through STRIDE; however, was unsuccessful. Will be attending school at Assumption High School in Wisconsin Rapids, WI in Fall 2025
Previously attended Auburndale High School but left due bullying
Struggles with spelling, math and science
Has been told previously to kill himself by other students from Auburndale
Entering 10th grade
Favorite subjects are science and history
Unsure about continuing education after graduatingQuit his job as a detailers TJ’s auto, currently unemployed
States his dream job would be working in IT Legal History:In the past, I don't want to talk about it. I not. I didn't know better, distributing cp, this is not a good thing, SNAP:good painter, good technology,
OUTPUTTherapy Intake Note
1. Identifying Information and Reason for Visit
Client Name: Morgan [Last Name]
Date of Birth: [MM/DD/YYYY] (17 years old)
Date of Intake: [MM/DD/YYYY]
Gender: Male
Ethnicity: White
Living Situation: Resides on a hobby farm in Milladore with father Chris (54), mother Kathy (49), sister Golda (12), and brother Gus (20).
Reason for Visit: Morgan presents with concerns regarding family dynamics, feelings of anxiety related to social interactions, and a fear of being kicked out of the house when he turns 18.
2. Presenting Problems
Onset and Duration: Morgan's concerns have been ongoing, influenced by family dynamics and prior bullying experiences.
Triggers: Incidents of family entering his space without permission, perceived lack of privacy, and recollections of negative peer interactions at school.
Severity: Morgan expresses significant anxiety and feelings of isolation, describing himself as an introvert who struggles to engage socially.
Functional Impact: The described concerns contribute to Morgan’s withdrawal from social situations, difficulty in educational settings, and feelings of worthlessness, particularly exacerbated by past bullying experiences which led to suicidal ideation.
3. Psychosocial History
Family/Supports:
Morgan reports a close relationship with his aunt Heather and uncle Steve.
His relationship with sister Golda is described as improving but still “not the best.”
He maintains a good relationship with his father, who engages in activities like playing Warhammer to strengthen their bond.
Morgan feels that his relationship with his mother is “iffy.”
Education/Work:
Currently enrolled in online schooling through STRIDE but was previously unsuccessful.
Morgan will attend Assumption High School starting Fall 2025.
He has previously attended Auburndale High School but left due to bullying which significantly impacted his academic performance.
Currently unemployed after quitting a job as a detailer at TJ’s Auto.
Living Situation: Morgan has his own room on the family farm but expresses feeling isolated.
Cultural Factors: Morgan reports no spiritual beliefs.
4. Relevant Medical and Psychiatric History
Medical Conditions: Morgan is underweight for his age with no other medical concerns reported.
Current Medications:
Duloxetine 30 mg (antidepressant)
Aripiprazole 2 mg (antipsychotic)
Prior Diagnoses/Treatment Response: Specific diagnoses were not disclosed; however, Morgan has a history of bullying leading to suicidal thoughts. He is currently receiving medication as part of a treatment plan.
5. Substance Use
Morgan reports no issues with substance use at the time of intake.
6. Risk Assessment and Safety Plan
Self-harm/Suicidal Ideation: Morgan has a history of suicidal ideation related to bullying experiences. No current suicidal thoughts reported during intake.
Protective Factors:
Supportive relationships with his father, aunt, and uncle.
Interest in engaging in activities such as Warhammer with his father.
Desire to improve social skills and become more outgoing.
Safety Plan: Collaboration with Morgan to create a plan involving safe coping strategies, identifying warning signs, and emergency contacts if feelings of distress arise.
7. Clinical Impressions
Morgan presents with symptoms consistent with anxiety and possible depression stemming from social isolation and trauma related to past experiences with bullying. His concerns around family dynamics and fear of abandonment further complicate his mental health state. A provisional diagnosis may include Generalized Anxiety Disorder (GAD) and Adjustment Disorder (with anxiety).
8. Client Goals and Initial Treatment Plan
Goals:
Develop social skills and decrease anxiety in social situations.
Improve familial communication and boundaries.
Enhance coping strategies to manage anxiety and fear of abandonment.
Initial Treatment Plan:
Frequency of sessions: Weekly individual therapy.
Modalities: Cognitive Behavioral Therapy (CBT) to address negative thought patterns, and Social Skills Training to bolster interactions.
Homework/Next Steps:
Morgan will maintain a daily log of social interactions and feelings associated with them.
Develop a list of personal boundaries he wishes to communicate with family members.
Explore interests in IT and identify actionable steps toward pursuing this career path.
Signature:
[Your Name, Credentials]
[Your Title]
[Date] - INPUT
Session information: CIS Reese, Specialist Sabir, and Intern Czerwinski arrived at Ct's home for a Crisis Assessment. Client presents with the issue of "I've been sick for a while", "I feel like I want to hurt myself", and "I need help, I'm in denial". Client says she lost her job in Georgia due to issues with work performance, being picked on and harassed, and being hurt at work and filing for worker's compensation. Client says after the job lost that she moved to Ohio to live with her sister. Client also says she has lost people she was close to recently and that that has been painful for her. Client says she has been "going to places I'm not supposed to" while she drinks and continues to consume alcohol. She states that she does this to isolate herself. Client says she has also been physically and mentally abused as both a child and as an adult. Client says "When I look in the mirror I see nobody". Client says she experiences daily depressed mood for most of the day, diminished interest or pleasure nearly all activities, significant weight gain, Insomnia, trouble walking and moving around, Fatigue, Feelings of worthlessness, Diminished ability to think or concentrate nearly every day, and Recurrent thoughts of harming herself. Client says she was hospitalized for a suicide attempt a few years ago and saw a provider - Christen Cochran FNP-C. She was unable to provide a diagnosis. She said that for a long time now and as recent as Sunday night that she has been using Benadryl to self medicate her insomnia. She says she experiences racing thoughts, impulsivity, risk taking, and irritability. She says she has had panic attacks in the past and currently has multiple worries. Seems to have a persecutory delusion that after her worker's compensation claim, she got back to working, and everyone at her job was gossiping about her and trying to have her fired. Client says she is drinking "everyday, all-day." and that she started drinking, like how she is now, 12 or 13 years ago but that she has been drinking alcohol for a "long time". Client also mentioned that she started drinking 10 years ago so client seems to be a poor historian. Suicide risk is moderate due to the excessive substance intake. Client, aged 59, is wearing a black shirt, blue pants, red GUESS brand shoes. She is a black female, hygine seems good, no odor, hair looks washed and well kept, Ct's clothes seem clean. Client says she would be interested in an impatient clinic and says that by going she can “get away from people” and ”get some help”. suicide RISK and protective FACTORS: She does have Hx of a significant attempt, she has a positive support system, she has had multiple recent losses, Acute anxiety is present, perceived sense of being a burden is present, Active substance use, no Family hx suicide, she lives with her sister, no Access to lethal means, no Command AH to harm self/others, no Recent discharge from hospital. Ct has never served in a war zone, client has been in a serious accident at work, Ct has never been in a major disaster, no life-threatening illnesses, Ct reports physical and mental abuse before 18, Ct has not been attacked or beaten by others, ct has been in situations where she felt her life was at risk and has had family members die violently, but has never witnessed death first hand. Ct does not appear to be at risk of violence or exploitation of others. Ct does report multiple medical concerns including anemia, VB12 deficiency, kidney stones, a past hysterectmy, and not being able to wear her glasses. Ct has never been convicted of a crime. Ct says she has a really hard time with lasting relationships because "people always leave me."
OUTPUTTherapy Intake Note
1. Identifying Information and Reason for Visit:
Client Name: Charlotte Jane Willis
Date of Birth: 4/23/1966
Age: 59
Gender: Female
Ethnicity: Black
Date of Assessment: [Insert Date of Assessment]
Referring Individual: Pamela Harris (Sister)
Reason for Visit: Client presented for a crisis assessment due to self-reported suicidal ideation, feelings of worthlessness, and persistent substance use. Client expressed a desire for help and indicated being in denial regarding her mental health and substance use issues.
2. Presenting Problems:
Onset: Concerns began escalating approximately 12-13 years ago with increased alcohol use and feelings of worthlessness.
Duration: Client reports daily depressive symptoms and recurrent thoughts of self-harm over the last several months.
Triggers: Recent job loss, multiple bereavements (including two brothers), and perceived harassment at previous employment.
Severity: Client reported moderate suicide risk due to excessive alcohol consumption and significant emotional distress.
Functional Impact: Limited ability to engage in daily activities, reported sleeping only 3-4 hours per night, and a diminished interest in previously enjoyed activities. Client is currently living with her sister but is reportedly at risk of homelessness if she does not seek treatment.
3. Psychosocial History:
Family/Supports: Client lives with her sister Pamela Harris, and another sister, Felita. Reported feelings of being a burden to her family. Strong support system identified, including her children.
Education/Work: Client has lost her job in Georgia due to performance issues and harassment, has been in Ohio for one month. Previous social drinker status reported, with recent change to daily drinking.
Living Situation: Currently residing with sister; however, expressed concerns regarding acceptance in the household if she does not comply with treatment recommendations.
Cultural Factors: Client has articulated a strong faith in God, although feels her prayers are unanswered, which contributes to feelings of hopelessness.
4. Relevant Medical and Psychiatric History:
Medications: Client reports using Benadryl for insomnia, no current prescribed medications known.
Prior Diagnoses: Client has a self-reported history of bipolar disorder but cannot specify further details.
Treatment Response: Client has a history of hospitalization due to a suicide attempt. Previous mental health treatment history is unclear.
5. Substance Use:
Client reports alcohol use beginning approximately 10 years ago, escalating to daily use over the last few years. Describes drinking "every day, all day," with Budweiser as her drink of choice.
Client reports being unable to recall specifics regarding frequency and quantity of use, indicating possible disorganization and denial.
6. Risk Assessment and Safety Plan:
Suicidal Ideation: Client endorses recurrent thoughts of self-harm but denies a specific plan or intent at this time.
Protective Factors: Client has children and responsive siblings as potential protective factors. Expressed interest in inpatient treatment as a means of safety and recovery.
Access to Means: Client has no access to lethal means such as firearms.
Current Risk: Moderate risk due to recent alcohol consumption and expressed feelings of worthlessness. Recommended immediate transport to inpatient facility for further assessment and safety stabilization.
7. Clinical Impressions and Provisional Diagnosis:
Client exhibits signs consistent with Major Depressive Disorder, including anhedonia, insomnia, feelings of worthlessness, and suicidal ideation. Possible co-occurring Substance Use Disorder related to alcohol use is indicated.
Provisional Diagnosis: Major Depressive Disorder (MDD) and Alcohol Use Disorder (AUD), pending further evaluation.
8. Client Goals and Initial Treatment Plan:
Client expressed a desire to enter an inpatient facility to undergo detox and receive a comprehensive mental health evaluation.
Initial Plan:
Transport client to Highland Springs for an immediate assessment.
Facilitate connection with case management for ongoing support during inpatient stay.
Recommend follow-up appointments post-discharge for continued mental health and substance abuse treatment.
Discuss potential outpatient therapy options to address long-term recovery and coping strategies.
Frequency of sessions to be determined based on client’s needs following assessment results.
Encourage client to journal or reflect on feelings and experiences during treatment for self-awareness and integration in therapy.
Signature:
[Your Name], LCSW
[Your Title / Credentials]
[Date]
Check out these other templatesSee all →
Therapy Practice Name Generator
Generate unique and meaningful names for your therapy practice or mental health clinic.
Clear, concise and authentic writing that gets your message across effectively.
Generate creative and engaging text for any purpose with our AI-powered text generator
Humanize AI Text To Bypass AI Detection
Transform AI-generated text to make it more human-like and bypass AI detection.
Generate compelling meta descriptions to improve click-through rates from search results.
Create Faster With AI.
Try it Risk-Free.
Stop wasting time and start creating high-quality content immediately with power of generative AI.